A Definitive Guide To Getting Pregnant With Donated Eggs
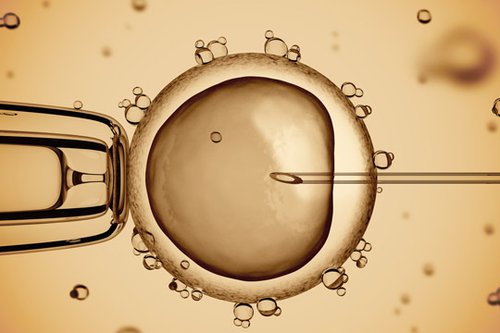
Egg donation is defined as the process where a woman’s ovaries are stimulated to produce multiple mature eggs, which are then harvested and donated, usually for the purpose of assisted or third party reproduction. Eggs may be frozen for later use or fertilized in vitro (in a laboratory).
Though initially beset by controversy, the science behind in vitro fertilization (IVF) and oocyte (egg) and embryo donation has completely changed the future of reproductive medicine and provided a new platform for advancements in women’s health.
Today, it is about women (the donors) helping people (of all orientations and relationship statuses) to overcome infertility challenges with the aid of technology.
In the decades since the first IVF pregnancy and subsequent birth, egg and embryo donation have become as commonplace as major organ donation. Women may choose to become an egg donor for any number of reasons, and the donated eggs can then be fertilized and implanted immediately or frozen for later use.
Research tells us that egg quality and quantity are closely related to a woman’s age. Women are born with all the eggs they will ever have and their quantity decreases over time. A woman’s fertility generally begins to decline in her mid-thirties and continues to accelerate. Though the woman may still be fertile, the quantity of available eggs decreases and the quality of the available eggs drops. Chromosomal abnormalities also increase markedly with age and women who wish to have children later in life may require the exploration of other options for becoming pregnant. At this stage, some women may explore the possibility of donor egg IVF, either by seeking out a fresh egg donor through a local program or utilizing a frozen egg bank.
Up until recently, fresh eggs were the preferred source for use in assisted reproductive technology (ART) and are still the most prevalent method used around the world. Recent advances in the way eggs are frozen and thawed; however, have led to frozen egg donation becoming a more viable option, and to the creation of companies like Donor Egg Bank USA (DEB USA) who offer a nationwide database of frozen donor eggs. The results are now more consistent and predictable than they have been in the past with clinics reporting excellent pregnancy and live birth success using frozen eggs. There are several advantages to choosing frozen eggs over fresh. Some of these include:
-
Synchronization of cycles between donor and recipient is unnecessary with frozen donor eggs
-
Any complications that may arise from ovarian stimulation have already been resolved, so this is one less area of stress for the patient
-
Costs are greatly reduced per treatment cycle using frozen over fresh eggs
-
The time involved in choosing/locating a suitable donor is reduced
-
Treatments can begin right away and are not dependent on the donor’s immediate health or availability
-
Additional frozen eggs may be available for siblings without the donor completing a new cycle
A Brief History of ART & Egg Donation
ART has advanced in stages, with the earliest reported attempt dating back to 1790 when a Scottish doctor inseminated a woman with her husband’s sperm. Nearly one hundred years later, in 1884, a woman was inseminated with donor sperm.
In 1944, pioneering physicians John Rock and Miriam Menkin reported the first in vitro fertilization of a human egg, though no pregnancy resulted.
In 1954, we saw the first successful pregnancy using frozen sperm and in 1978, the first baby conceived through IVF was born.
The first pregnancy from a donated egg was reported in Australia in 1983, while the first successful birth occurred one year later in California, the result of a procedure that transplanted an already-fertilized egg from one woman to another. Performed at UCLA Medical Center, the birth heralded a new era for single women, infertile couples and same-sex couples who wished to start a family. Prior to this breakthrough, the only option available to these parental hopefuls was adoption or surrogacy. For women who were unable to become pregnant or who were at risk of passing on various genetic disorders, this new approach opened the doors to exciting new possibilities.
More Recently
Since that first birth from a donated egg, there have been more than 50,000 live births from donated eggs. As the practice became more widespread, much legislation has been debated and passed into law. The American Society for Reproductive Medicine (ASRM) established guidelines for the procedures involved, as did the Food and Drug Administration. As a result, many women travel to the US from foreign countries that do not allow compensation of an egg donor’s time and inconvenience. For many donors, the practice is purely altruistic, but it can also provide some attractive financial benefits.
The development of frozen egg donation was initially fraught with challenges. Early attempts used a slow-freeze method, which didn’t produce reliable results. After the discovery of vitrification, or flash freezing, success rates greatly improved and it finally became a viable solution. And for women who weren’t ready to start a family in their younger, more fertile years, it allowed them to freeze their own eggs to be thawed at a time of their choosing.
In 2012, the ASRM recognized that the process of egg freezing resulted in an ‘acceptable’ percentage of births, enough for them to remove the ‘experimental’ label on the procedure. Currently, at programs skilled in the technological technique, there is an equal chance of a successful pregnancy from frozen eggs as there is with women undergoing IVF using fresh eggs.
Indications for Donor Eggs
The typical recipient of donor eggs can be categorized into several subsets:
-
Women who have previously had multiple unsuccessful in-vitro treatments. Poor egg quality and genetic abnormalities may be a contributing factor in the failure to conceive by this method.
-
Secondary infertility, defined as when one child is conceived naturally but a second attempt is unsuccessful. There can be many causes of secondary infertility including age, structural complications such as endometriosis, sperm quality and quantity, weight gain and smoking.
-
Premature ovarian failure (menopause before the age of forty).
-
Women affected by reproductive abnormalities that would cause them to not produce viable eggs.
-
Male same sex couples.
-
Other unexplained infertility issues.
For recipients of donor eggs, the question becomes: fresh or frozen? There are distinct steps towards success in each of these cases. The decision involves the determination of which process is right for each individual. The cycle for frozen egg IVF is much less complicated and has a range of advantages that run the gamut between physical, psychological, legal and financial. The cycle time is also greatly shortened using frozen eggs and recipients have more flexibility in terms of scheduling each step of the procedure.
Preparation for Egg Recipients
A full medical evaluation is necessary for all women who hope to conceive using donor eggs.

A complete physical exam should conclude that their health will not be significantly jeopardized by a pregnancy. A full range of testing may include a cervical culture, a hysteroscopy and a hysterosalpingogram or saline sonogram to assess uterine health. Semen testing should also be performed on the male counterpart to rule out any contributing factors. Some clinics will order a course of hormone replacement prior to the actual embryo transfer: called a ‘prep’, ‘mock’ or ‘dummy’ cycle, it is used to ensure that the hormonal treatment will achieve the desired blood levels and endometrial effects. Some doctors will elect to perform an endometrial biopsy during this cycle to measure the thickness of the endometrial stripe. Preparations should always include a thorough explanation and discussion of the procedural aspects as well as an exploration of the psychological and social impacts of third party reproduction.
Not all women need an egg donor and if she is still young enough personal egg freezing may still be indicated. Of the women who are physiologically able to conceive, some prefer to take control of the event and make it happen at a time of their own choosing. Depending on the individual situation, many women are choosing to freeze their eggs while they are in their twenties or thirties, the age at which eggs are considered to be the highest quality and most viable. Eggs are retrieved in the same surgical procedure as egg donation and similarly are frozen for use at a later date. For those women who froze their eggs in their younger years and are unsuccessful, donor eggs could still become part of their future journey.
Egg Donation Risks
Of course, as with all medical procedures, minor risks should be considered when electing to pursue donor egg IVF. Whether you are choosing to use fresh or frozen donor eggs, there is about a 50% chance that any given cycle will result in a pregnancy. There is also a possibility of a pregnancy with multiple babies, which carries the added potential for premature delivery, low birth weight, miscarriage or developmental difficulties in the child, and raised blood pressure or gestational diabetes for the mother. Because of this, most physicians will not implant more than two embryos at one time.
The process for fresh donated eggs is increasingly unpredictable, as it involves two separate individuals: the recipient of the eggs and the donor who produces them. In this case, the risks are doubled as certain conditions must be met in both cases. The greatest risk in a fresh donation cycle is the donor becomes disqualified to move forward. There is extensive testing that must be performed in accordance with the US Federal Drug Administration requirements. All donors who test positive are disqualified from moving forward. Egg donors also receive a psychological test as well as a visit with a social worker. Programs such as Donor Egg Bank USA require genetic testing and a thorough visit with a physician or physician assistant/nurse practitioner which includes blood work and a physical exam. At any point in the process, the donor may change her mind or it may be determined that she is not an acceptable candidate for egg donation. Typically, in a fresh donation process, the recipient bears the financial burden of a donor who is not qualified to move forward. Sometimes disqualification of an egg donor can happen several times before a couple identifies a donor who is deemed appropriate to move forward.
The process for frozen donor eggs is less risky because the eggs are already frozen and the egg donor has completed her cycle. Risks of disqualification are nearly zero giving the egg recipient comfort in knowing that the egg donor chosen will have eggs available to move forward with a cycle. Removing the risk associated with the donor’s cycle minimizes the time between donor choice and treatment by as much as four to nine months.
How Much do Fresh and Frozen Donor Eggs Cost?
Frozen egg donation and the implantation procedure can be accomplished at about half the cost of a fresh donor egg cycle. The total cost of a fresh cycle can be as high as $30 - $40K when donor recruitment, screening, preparation, treatment, medication and after-care for both donor and recipient are considered. In contrast, the total cost of a frozen egg cycle is in the range of $15 - $21K. There are numerous differences between the two processes which account for the significant difference in cost.
IVF with Fresh Donor Eggs: The Process
If you are considering going the route of using fresh donor eggs, here is a detailed journey of what you should expect:
-
Search for an egg donor: Many individuals work with an agency which can cost between $5,000 and $8,000 per cycle to recruit an egg donor. Depending on the unique requirements for the donor (e.g., race, eye color, etc.…), this process could take anywhere from one month to several months.
-
Contracts and attorney visit: Once an egg donor is found a contract between the individual and donor is put in place to ensure the rights of the recipient and to relinquish the eggs and ultimate baby from the donor. Typically, this step will involve an attorney.
-
Egg donor testing: The egg donor will then begin her evaluation with base line hormonal testing to determine her suitability to be a donor. She will receive psychological testing, a visit with a social worker or psychologist and genetic testing. She will have a full medical history review and physical completed to ensure she is healthy to perform the donation. At any step, the donor could be disqualified and the recipient may need to start again adding to their financial expenditure.
-
Mandatory infectious disease testing: All donors are required to have infectious disease testing as determined by the FDA. A positive test and the donor will be disqualified.
-
Recipient workup: The recipient will also receive a full medical evaluation to include a complete physical and psychological workup to determine any risk factors. Tests for the female recipient could include a cervical culture, a hysteroscopy and a hysterosalpingogram or saline sonogram to assess uterine health. The recipient work-up can take three months to complete if the individual is motivated and more if the process if followed leisurely.
-
‘Prep Cycle’ or ‘Mock Cycle’: This cycle is usually coupled with a trial transfer and is a course of hormonal therapy that ensures that the treatment will achieve the desired blood levels and endometrial effects. Some doctors will elect to perform an endometrial biopsy during this cycle to measure the thickness of the endometrial stripe. Typically, a trial transfer is performed during a mock cycle. This procedure is used to discover uterine depth and to ensure the physician can navigate the catheter to just the right spot in the uterus. The mock cycle must be timed with a woman’s cycle and takes only 15 days to complete once her cycle starts.
-
Suppression of the normal menstrual cycle and stimulation: The egg donor is given birth control pills to suppress her menstrual cycle and to synchronize it with a recipient. She will receive hormones as a daily, self-administered injection. This phase lasts about two weeks and the donor is monitored through blood tests and ultrasound during this time.
-
Endometrial lining development for the recipient: While the donor is taking hormones to boost her egg supply, the recipient takes a combination of first estrogen and then progesterone to prepare the uterus for a successful implantation. Patients with autoimmune issues may require additional medications. Most physician protocols require 12 – 14 days of estrogen prior to triggering ovulation.
-
Triggering ovulation and egg retrieval: When an ultrasound determines that the eggs have developed sufficiently, the donor will trigger ovulation with an injection of hCG. After thirty-six hours, the eggs are retrieved in a short procedure, performed under intra-venous sedation. It is a trans-vaginal procedure using an aspiration needle, guided by ultrasound.
-
Fertilization and transfer of the embryo: Eggs are retrieved and fertilized with donor sperm or the partner’s sperm. In the latter case, the partner will be required to visit the office to provide a sample. Embryos from this phase are then incubated and generally implanted in the recipient on either the third or fifth day after fertilization.
-
Post retrieval check-up: The donor returns to the office to be evaluated to ensure a full recovery from the procedure. In most cases, the donor can return to normal activity in a day or two after egg retrieval. For most donors, and without extenuating circumstances, the entire process will take about three to five weeks.
-
Post-implantation check-up: Recipients will have a pregnancy test two weeks after implantation. This is accomplished with a blood test that measures the pregnancy hormone hCG. Once the pregnancy has been confirmed via two rising hCG tests and an ultrasound which looks for the baby’s heartbeat, the recipient is discharged to their OB/GYN for prenatal care.
IVF with Frozen Donor Eggs: The Process
The process for IVF using frozen eggs is much less complicated, as the donor has already completed her half of the process. Eggs are already collected and ready for fertilization.
-
Full medical evaluation: Recipient undergoes a complete physical and psychological workup to determine any risk factors. Tests could include a cervical culture, a hysteroscopy, hysterosalpingogram or saline sonogram to assess uterine health.
-
‘Prep Cycle’ or ‘Mock Cycle’: An optional course of hormonal therapy that ensures that the treatment will achieve the desired blood levels and endometrial effects. Doctors may perform an endometrial biopsy during this cycle to measure the thickness of the endometrial stripe. As well, a trial transfer may be completed to practice for the big event.
-
Endometrial lining development: The recipient will take a combination of first estrogen and then progesterone to prepare the uterus for a successful implantation. Patients with autoimmune issues may require additional medications.
-
Fertilization, incubation and transfer of the embryo: Eggs are thawed and fertilized with donor sperm or the partner’s sperm. In the latter case, the partner will be required to visit the office to provide a sample. Embryos from this phase are then incubated and generally implanted in the recipient on either the third or fifth day after fertilization.
-
Pregnancy test: Recipients will have a pregnancy test two weeks after implantation. This is accomplished with a blood test that measures the pregnancy hormone hCG. Once the pregnancy has been confirmed via two rising hCG tests and an ultrasound to detect the baby’s heartbeat, they are discharged to their OB/GYN for prenatal care.
What is the Profile of an Egg Donor?
Each egg donor has a different reason for choosing to be a donor. For the vast majority of donors, it is an altruistic endeavor, while for a few others, it is the promise of a financial payment. Why does a donor donate? Typically, she is drawn to make a donation because she knows someone who has struggled to have a baby or perhaps she has chosen to abort a baby and is seeking some level of atonement. Many donors are mothers themselves and can’t imagine life without their children. Giving the gift of life is powerful motivator and helping others in need is self-fulfilling.
Donors who enter the process for only financial gain are quickly dismayed at the time commitment and physical requirements to be a donor. These women will often drop out during the process as the financial gain does not always fully compensate for the time and inconvenience. For those that continue on, typically the motivating factor is the desire to further their education and the compensation makes additional schooling possible.
Not just anyone can be an egg donor. There are several requirements that screen out donors to include medical physical examinations, drug screening, multi-generational medical history screening, genetics screening and an in-depth psychological evaluation and test is performed to ensure that only appropriate candidates advance to the donation phase. In addition, each potential donor must submit an application that provides information on work history, education and personal background. This information is provided to the recipient in order to give them the opportunity to make the best possible choice for their family. It should be noted that the donor is relied upon to provide truthful information. Because of today’s health protection laws and privacy laws, DEB USA is unable to validate the truthfulness of the donor’s responses.
Legal Issues Surrounding Donated Eggs
Fresh egg donation carries a range of legal implications and greater potential risk as compared with frozen eggs.

Frozen eggs from an anonymous donor virtually eliminates the need for legal counsel as the donor has completed her cycle and relinquished her eggs.
If a ‘known’ donor is in the picture, an attorney is highly recommended – preferably one who specializes in reproductive law. Proceeding without a legal agreement in this case can put much at risk, including challenges to parenting, financial disputes, rights, responsibilities, obligations, contact, presumption of parentage and most importantly, parental rights. The presumption of parentage on the part of the donor should be effectively relinquished and this is best accomplished with a sound donor agreement. Additional issues could include the disposition of excess embryos and insurance issues, such as denial of payment. Generally, this aspect is the onus of the intended parents, as it is in their best interests to protect their donor conceived child against any future disputes. However, the donor may also be interested in protecting herself from liability should unforeseen circumstances arise.
When agreements are sound, the intended parents are acknowledged as the legal parents with every parental right that is implicated. The donor is also protected and her rights or lack thereof are spelled out for the future. It is always a good idea to pursue legal counsel as soon as the decision is made to pursue this course of action.
To Tell or Not to Tell
The decision to use a donor’s egg to achieve a family is an important one and typically private.

Current research suggests that children told about their genetic origins while young fair better going into adulthood. Nonetheless, no one can force the intended parent to tell their child and the implications of this decision should be weighed, particularly as it relates to the medical history of the child and future medical treatment decisions which could be contradicted or enhanced if the donor’s history were known. Making the decision to not tell should be researched and decided with caution knowing the future risks.
Some intended parents not only intend to tell their children but also desire open relationships with the donor. ID Disclosure release programs in which the donor has agreed to a mediated meeting at the age of majority are now available. If this is important to the intended parent, then a donor who has opted into this program is a better fit over a donor who has not elected to participate.
The Donor Sibling Registry is also a great resource for donors and intended parents who wish to meet. Registry is a nominal fee and each party can individually place their information on-line with the hope of a future match. Many half siblings have been found through the registry.
Single Women and LGBT Communities Benefit from Egg Donation
While there are many couples that can benefit greatly from donated eggs, it also serves as a family building option for women who wish to be a single parent and those in the LGBT community.

The ability to build a family with a biological connection, as opposed to adoption, is an exciting option for both communities. Increasingly women over the age of 40 who may not have found Mr. Right are “having it all” on their own terms. Using a combination of donor egg and donor sperm, these women are conceiving and birthing children at historical rates. In addition, egg donation has been revolutionary in the same sex community and men having babies through the use of a gestational carrier is on the rise.
Meanwhile, lesbian couples are using donor eggs; sharing the pregnancy with one being the donor and the other the carrier. With the added family security that comes with the legalization of same-sex marriage, many couples are becoming more interested in building their family unit within the institution of marriage. For LGBT couples, egg donation is a happy and exciting process, as opposed to heterosexual couples, where it often comes after years of inability to conceive. But the common ground between them all is the desire to have a healthy child.
What Egg Donors and Recipients Should Look Forward To
The process of egg donation is two-fold: for egg donors, it is a chance to help others achieve their most cherished dreams. For the egg recipients, it is a chance to conceive, start a family and complete a picture of happiness. Essentially, it is making the impossible possible.
There are several questions that concern many couples considering donated eggs that include whether the recipient will truly feel that the child is theirs, how can they approach the inevitable discussion about how the conception took place and several others. These are great questions to discuss with a reproductive psychologist. Many women and men have conceived via donor egg IVF and the good news is there is a community of supporters at Parent’s Via Egg Donation (PVED) who are willing to help intended parents navigate these tricky questions. As for will the baby feel like yours? Click our video to find out.
You might say that the donor is the genetic contributor, but the person who carried the child is truly the biological mother.
While there is a delicate balance to be struck, one fact remains: this child was brought into the world with great thought, love and intent from many sources.
The Role of DEB USA in the Egg Donation Process
DEB USA is a network of the most respected and established fertility clinics in the United States and Canada. With the most diverse database of egg donors and its high rate of success, DEB USA is North America’s preferred donor egg bank. With comprehensive 100% money back guarantee plans and the industry’s most competitive financial packages, DEB USA is the number one choice for collaborative family planning.
If you have been thinking about donor egg IVF for yourself or a friend or if you are wondering if you would be a good egg donor candidate, call or contact us today. It’s about your future, the way you envision it.